Can laser surgery for hemorrhoids be avoided and perhaps treated with a natural remedy?
If you have got to the point of considering laser surgery first understand what you hemorrhoids are and how they can be classified and treated using surgical and non surgical methods. After you have consulted a medical practitioner who understands the field then you may consider to opt for trying a non-surgical approach first before going for a surgical solution which may leave you with more problems such as weak bladder control.
Surgery for any reason comes with risks and if you have no health insurance or live in a country without a national health service it may be very expensive. Always consult a medical practitioner to make sure firstly you actually have hemorrhoids and no some other problem that is giving a similar appearance or symptoms also to talk over any non surgical options that may be worth trying first.
Surgery Techniques For Hemorrhoids
- Milligan-Morgan: The three major hemorrhoidal vessels are excised. Three pear-shaped incisions are left open to avoid stenosis and are separated by small bridges of mucosa and skin.
- Stapled Hemorrhoidopexy (PPH Procedure): This is a relatively new technique that reduces the prolapse of the hemorrhoidal tissue. This is accomplished by excising a band of the prolapsed anal mucosa membrane by using a circular stapling device. The stapling device is Circular Anal Dilator, it is responsible for the reduction of the prolapse of the anal skin and some parts of the anal mucous membrane. Then follows the Purse-String Anoscope, it pushes the mucous prolapse back against the rectal wall.
- Harmonic Scalpel For Hemorrhoids: This device uses ultrasonic technology. Ultrasonic treatment allows for both cutting and coagulation of hemorrhoidal tissue precisely at the point of application. This causes minimal thermal damage to the tissue.
- Laser Surgery For Hemorrhoids: Unwanted hemorrhoids are vaporized and excised. Considered the most precise of the surgical options. Because of this the procedures are more quickly completed and with less difficulty for the patient and doctor. This can be either the primary procedure or used in combination with other modalities.
- Atomizing Hemorrhoids: This is a new technique. The Atomizer is a medical device designed for tissue atomization. This basically means that hemorrhoids are reduced to minute particles much like a mist that is then vacuumed away. This is accomplished with an waveform of electrical current and a specialized electrical probe, the Atomizer Wand. The Atomizer Wand vaporizes the cell layers one or more at a time. Hemorrhoids are essentially disintegrated into an aerosol of carbon and water molecules. The Atomizer can also sculpt the tissue into a desired shape and smoothness.
Evaluation of Hemorrhoids
The evaluation of hemorrhoids should include a problem-specific history and physical examination: Level of Evidence, Class V; Grade of Recommendation, D.
A targeted history and physical examination is the initial step in the evaluation of the patient with hemorrhoids. In addition to the nature, duration, and severity of symptoms, the history should include an assessment of dietary fiber intake and bowel habits. In patients with rectal bleeding, a family medical history is needed to evaluate the possibility of familial colorectal neoplastic syndromes and the need for more extensive colon evaluation. The physical examination should typically include visual inspection of the anus, digital rectal examination, and anoscopy. The grade of hemorrhoidal disease can be classified using the definitions in the table below. Laboratory evaluation is not typically required.
Table: Classification of Internal Hemorrhoids
Classification Of Hemorrhoids
Grade Physical Findings
I Prominent hemorrhoidal vessels, no prolapse
II Prolapse with Valsalva and spontaneous reduction
III Prolapse with Valsalva requires manual reduction
IV Chronically prolapsed manual reduction ineffective
Evaluation of Rectal Bleeding
Complete colon evaluation with colonoscopy or barium enema with flexible sigmoidoscopy is typically indicated for patients with rectal bleeding who meet specific criteria: Level of Evidence, Class II; Grade of Recommendation, B.
The primary concern of patients with rectal bleeding is the possibility of colorectal neoplasia. Other diagnoses that may need to be excluded include inflammatory bowel disease, other forms of colitis, diverticular disease, and angiodysplasia. A careful history and physical examination are the cornerstones of appropriate use of endoscopic procedures, which may include proctoscopy and/or flexible sigmoidoscopy. More extensive endoscopic evaluation with complete colonoscopy or flexible sigmoidoscopy combined with barium enema is indicated for those who fulfill the criteria in the table below.
Table: Indications for Complete Colon Evaluation
* Age >50 years if no complete examination within 10 years
* >40 years with history positive for a single, first-degree relative with colorectal cancer or adenoma diagnosed at age >60 and no complete examination with 10 years
* >50 years if the history is positive for two or more first-degree relatives with colorectal cancer or adenomas diagnosed at age >60 and no complete examination within 3 to 5 years
* Positive fecal occult blood test
* Iron-deficiency anemia
Adapted from the Multi-Society Task Force on Colorectal Cancers
Medical Treatment for Hemorrhoids
Dietary management consisting of adequate fluid and fiber intake is the primary noninvasive treatment of symptomatic hemorrhoids: Level of Evidence, Class II; Grade of Recommendation, B.
The typical symptoms of internal hemorrhoids are rectal bleeding and prolapse. Nonoperative treatment is ineffective for hemorrhoids with significant prolapse (Grades III-IV) and consideration should be given to more aggressive treatment modalities. For hemorrhoids with lesser prolapse, dietary management with adequate fluid and fiber intake to avoid straining is effective.
Dietary management also is the primary modality in the treatment of hemorrhoidal bleeding.
Office Treatment
Most patients with refractory Grades I, II, or III hemorrhoids are candidates for office-based procedures. Hemorrhoid banding is usually the most effective option. Other options include sclerotherapy, infrared coagulation, bicap coagulation, and cryotherapy: Level of Evidence, Class I; Grade of Recommendation, B.
Office treatment of hemorrhoids includes several procedures, which all attempt to decrease vascularity, decrease hemorrhoidal volume, and increase fixation of the fibrovascular cushion to the rectal wall. This leads to improvement in the specific symptoms of prolapse and rectal bleeding.
A single hemorrhoid or multiple hemorrhoids may be ligated with rubber bands per session.
Sclerotherapy involves injecting a sclerosant into the apex of the hemorrhoid and is effective in 75 to 89 percent of patients with Grades I, II, and III hemorrhoids. This has been associated with slightly less pain than hemorrhoidal banding. It has been used in combination with rubber band ligation with increased success rates.
Infrared coagulation involves direct application of infrared waves resulting in protein necrosis. It is most applicable to Grades I and II hemorrhoids but is associated with high rates of recurrence when substantial prolapse is present.
The application of both direct current and bipolar current has proven useful in the treatment of Grades I to III hemorrhoids. Bicap (bipolar current) has the advantage that treatment application lasts only several seconds compared with eight to ten minutes per application for direct current. Both are associated with a minor complication rate of 10 percent and recurrence rates between 25 and 35 percent.
Cryotherapy uses cold coagulation to relieve symptoms.
The incidence of minor complications after the various office-based procedures is reasonably similar.
Thrombosed External Hemorrhoids
Treatment options include observation or excision; however, excision, within 48 to 72 hours of onset of symptoms, in the office setting under local anesthesia or occasionally in the operating room will result in the most rapid relief from symptoms: Level of Evidence, IV; Grade of Recommendation, B.
External hemorrhoids may thrombose spontaneously, possibly secondary to straining at stool or heavy lifting. The exact etiology remains unknown. There is little scientific data comparing treatment options for external hemorrhoidal thrombosis. Clinical experience leads to the recommendation that individuals with symptoms who present fewer than 48 to 72 hours will be best treated by local excision of the external component. This can commonly be performed in the office setting but may occasionally require treatment in the operating room because of large size, extension within the anal canal, or patient anxiety.
Thrombosis that has been present for more than 72 hours often can be treated expectantly if the pain is not too severe. In this circumstance, avoidance of constipation, patient analgesia, and ice or sitz baths to the perineum may result in more rapid symptom relief than will surgical excision. Simple incision and evacuation of the clot should be avoided, because the lesion is typically made up of multiple, small, intravascular thromboses rather than a single hematoma. Also, simple incision and drainage often results in rethrombosis at the original site and even extension to include circumferential hemorrhoidal thrombosis.
Surgical Hemorrhoidectomy
Hemorrhoidectomy should be reserved for patients refractory to office procedures or unable to tolerate office procedures, patients with large external hemorrhoids, or patients with combined internal and external hemorrhoids with significant prolapse (Grades III-IV): Level of Evidence, I; Grade of Recommendation, B.
Individual patient factors and preferences need to be carefully weighed and considered. Surgical options include open or closed hemorrhoidectomy performed with surgical scalpel, diathermy, laser, or ultrasonic scalpel. All are reasonable options with none having a clear advantage over any other.
Stapled hemorrhoidopexy is a new alternative available for individuals with significant hemorrhoidal prolapse. It involves a mucosal and submucosal, circular resection of the hemorrhoidal columns at their apex. In addition, the blood supply is interrupted and hemorrhoids are “fixed” to the distal rectal muscular wall. This is all accomplished by a single firing of a modified, circular anastomotic stapler. Exceptionally rare but potentially devastating complications include anovaginal fistula, substantial hemorrhage, fistula, retroperitoneal sepsis, and rectal perforation.
What are Hemorrhoids?
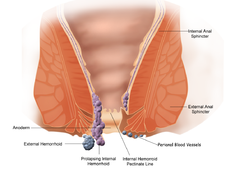
Hemorrhoids (US English) or haemorrhoids (Commonwealth English), also known as piles and “Tum-Bum”, are part of the normal human anatomy of the anal canal. They become pathological when swollen or inflamed. In their physiological state they act as cushions composed of arterio-venous channels and connective tissue that aid the passage of stool. The symptoms of pathological hemorrhoids depend on the type present. Internal hemorrhoids usually present with painless rectal bleeding while external hemorrhoids present with pain in the area of the anus.
Recommended treatment consists of increasing fiber intake, oral fluids to maintain hydration, NSAID analgesics, sitz baths, and rest. Surgery is reserved for those who fail to improve following these measures.
Signs and symptoms
Classical appearance of an external hemorrhoid.

External Herrhoid
Hemorrhoids are usually benign. In most cases, symptoms will resolve within a few days. External hemorrhoids are painful while internal hemorrhoids usually are not.

Internal Hemorrhoid
The most common symptom of internal hemorrhoids is bright red blood covering the stool, a condition known as hematochezia, on toilet paper, or in the toilet bowl. They may protrude through the anus. Symptoms of external hemorrhoids include painful swelling or lump around the anus.
Causes
A number of factors may lead to the formations of hemorrhoids including irregular bowel habits (constipation or diarrhea), exercise, gravity, nutrition (low-fiber diet), increased intra-abdominal pressure (prolonged straining), pregnancy, genetics, absence of valves within the hemorrhoidal veins, and aging.
Other factors that can increase the rectal vein pressure resulting in hemorrhoids include obesity, and sitting for long periods of time.
During pregnancy, pressure from the fetus on the abdomen and hormonal changes cause the hemorrhoidal vessels to enlarge. Delivery also leads to increase intra abdominal pressures. Surgical treatment is rarely needed as symptoms usually resolve post delivery.
Hemorrhoid cushions are a part of normal human anatomy and only become a pathological disease when they experience abnormal changes. There are three cushions present in the normal anal canal.
Prevention
The best way to prevent hemorrhoids is to keep stools soft so they pass easily, thus decreasing pressure and straining, and to empty bowels as soon as possible after the urge occurs. Exercise, including walking, and increased fiber in the diet help reduce constipation and straining by producing stools that are softer and easier to pass. Spending less time attempting to defecate and avoiding reading while on the toilet have been recommended.
Diagnosis
Endoscopic image of internal hemorrhoids seen on retroflexion of the flexible sigmoidoscope at the ano-rectal junction
A visual examination of the anus and surrounding area may be able to diagnose external or prolapsed hemorrhoids. A rectal exam may be performed to detect possible rectal tumors, polyps, an enlarged prostate, or abscesses. This examination may not be possible without appropriate sedation due to pain.
Visual confirmation of internal hemorrhoids is via anoscopy. This device is basically a hollow tube with a light attached at one end that allows one to see the internal hemorrhoids, as well possible polyps in the rectum.
Many anorectal problems, including fissures, fistulae, abscesses, colorectal cancer, rectal varices and itching,diverticulosis,polyps have similar symptoms and may be incorrectly referred to as hemorrhoids.
Treatments
Conservative treatment typically consists of increasing dietary fiber, oral fluids to maintain hydration, non-steroidal anti-inflammatory drugs (NSAID)s, sitz baths, and rest. Increased fiber intake has been shown to improve outcomes and may be achieved by dietary alterations or the consumption of fibre supplements.
While many topical agents and suppositories are available for the treatment of hemorrhoids there is little evidence to support their use. Preparation H may improve local symptoms but does not improve the underlying disorder and long term use is discouraged due to local irritation of the skin.
* Rubber band ligation is a procedure in which elastic bands are applied onto an internal hemorrhoid at least 1 cm above the dentate line to cut off its blood supply. Within 5–7 days, the withered hemorrhoid falls off. If the band is placed too close to the dentate line intense pain results immediately afterwards. Cure rate has been found to be about 87%.
* Sclerotherapy involves the injection of a sclerosing agent (such as phenol) into the hemorrhoid. This causes the vein walls to collapse and the hemorrhoids to shrivel up. The success rate at four years is 70%.
* A number of cautery methods have been shown to be effective for hemorrhoids. This can be done using electrocautery, infrared radiation, or cryosurgery.
A number of surgical techniques may be used if conservative medical management fails. All are associated with some degree of complications including urinary retention, due to the close proximity to the rectum of the nerves that supply the bladder, bleeding, infection, and anal strictures.
* Hemorrhoidectomy is a surgical excision of the hemorrhoid used primary only in severe cases. It is associated with significant post operative pain and usually requires 2–4 weeks for recovery.
* Doppler guided transanal hemorrhoidal dearterialization is a minimally invasive treatment using an ultrasound doppler to accurately locate the arterial blood inflow. These arteries are then “tied off” and the prolapsed tissue is sutured back to its normal position. It has a slightly higher recurrence rate however has less complications compared to a hemorrhoidectomy.
* Stapled hemorrhoidectomy is a procedure that involves resection of soft tissue proximal to the dentate line, disrupting the blood flow to the hemorrhoids. It is generally less painful than complete removal of hemorrhoids and was associated with faster healing compare to a hemorrhoidectomy.
References.
National Guidline clearinghouse
http://www.guideline.gov/summary/summary.aspx?ss=15&doc_id=7284&nbr=4337
Wikipedia
http://en.wikipedia.org/wiki/Hemorrhoid